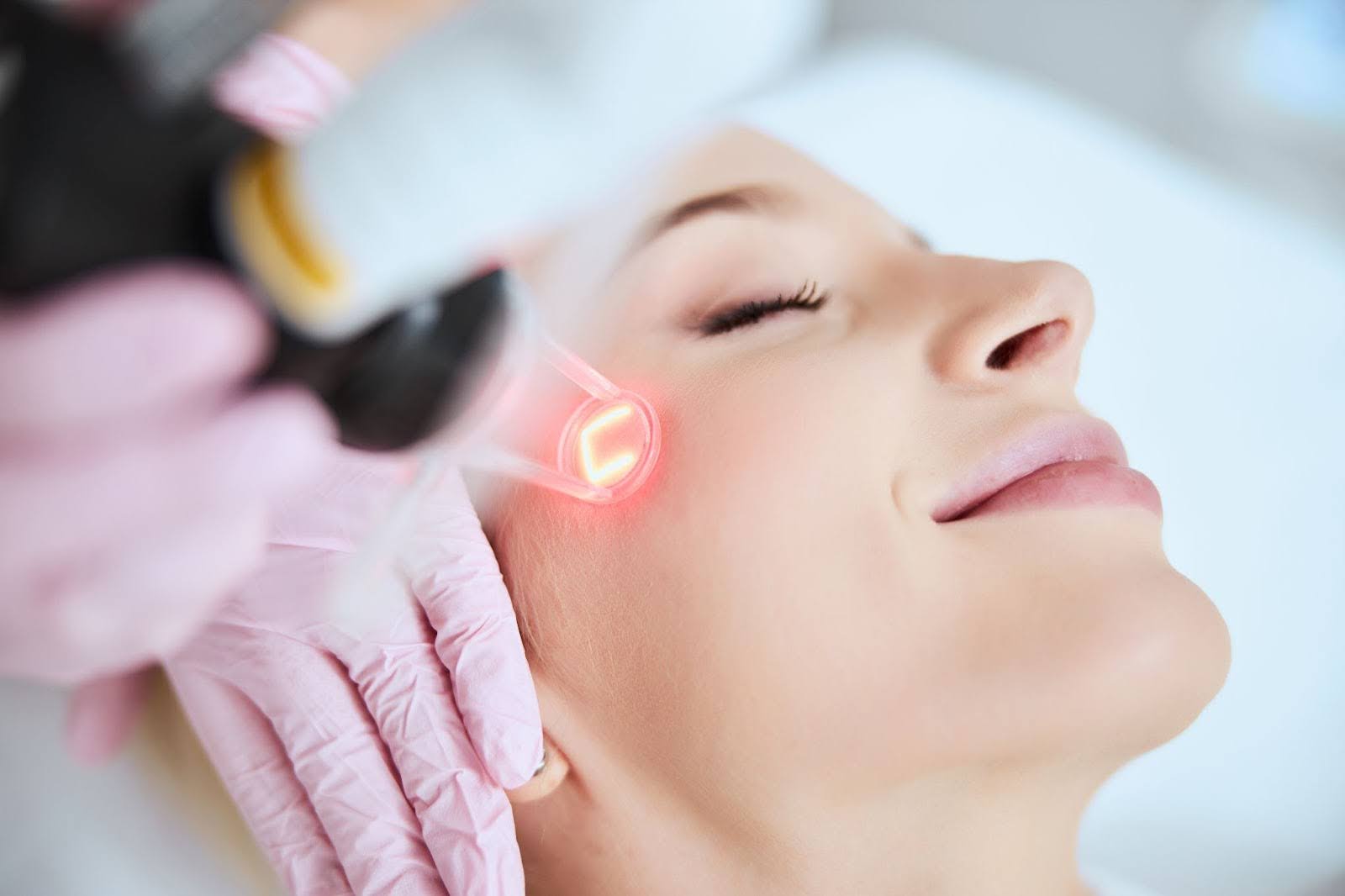
According to the American Board of Facial Cosmetic Surgery, CO2 laser skin resurfacing is one of the most sought-after cosmetic treatments. In 2021, more than 500,000 cosmetic treatments of this sort were performed.
Although it may sound futuristic, lasers are critical to modern medicine, and cosmetic surgeons have used them for decades. The technology keeps getting better.
That all sounds great, but what about the cost? For example, how much does CO2 laser skin resufacing treatment cost?
In most cases, CO2 laser treatment is an elective procedure. In other words, you are choosing it, and it is not medically necessary. That means most insurance plans will not cover it, so cost is a consideration. What does laser skin rejuvenation cost?

What is exactly CO2 Laser Treatment?
How Does CO2 Laser Treatment Work?
A CO2 laser treatment targets beams of light on the superficial layers of the skin to smooth it out and remove imperfections.
The laser energy of CO2 treatment can be effective for:
- Removing skin cancer
- Reducing the signs of aging, such as fine wrinkles and deep lines
- Reducing scarring or age spots to eliminate them or make them less noticeable
- Evening out uneven skin tone to eliminate sun damage or hyperpigmentation and other forms of discoloration
- Smooths out skin texture
- Treat varicose veins in the face and chest
- Eliminate dark circles under the eyes
- To promote younger skin growth
- Stimulate new skin cells
- Treat Rosacea
- Fade stretch marks
CO2 stands for carbon dioxide, and CO2 laser skin resurfacing represents one of the most significant breakthroughs in dermatology. Here’s What You Need to Know About Laser Skin Resurfacing for those considering this treatment.
Laser resurfacing deploys beams of light to remove the superficial layer of skin called the epidermis. With skin laser resurfacing, beams of light penetrate the skin. Water in the skin cells absorbs the light, heating up the middle layer. That heat vaporizes the epidermis. At the same time, the temperature rise stimulates collagen production, helping new skin grow,
Two primary types of CO2 lasers exist for cosmetic treatments:
- Ablative – Uses a pulsed laser to add energy to a continuous skin area. The energy increases the temperature of the water in the tissue, causing it to ablate or remove problem areas.
- Fractional – Uses many smaller or mini beams in the treatment area. Unlike the ablative device, the fractional laser applies the beam more sporadically instead of continuously, allowing for a more selectively focused application.
CO2 laser skin resurfacing provides smoother, healthier, and younger-looking skin.
What Are the Benefits of a CO2 Laser Skin Resurfacing Treatment?
CO2 laser therapy can target a variety of skin conditions and provide long-lasting results. The exact benefits depend on a variety of factors, such as:
- Skin type
- Pigmentation
- Underlying health conditions
- Type of laser
- The extent of skin issues
CO2 laser therapy effectively addresses various skin concerns, some of which are difficult to treat in other ways. Here’s what you need to know about CO2 Laser Skin Benefits.
Acne Scars and Blemishes
The intense pulsed light of a CO2 laser can break up scar tissue and stimulate the creation of new collagen. The new skin will help fill in scarred areas and lead to younger, healthier-looking skin.
Diminishing Wrinkles
Laser treatment ablates superficial skin layers, resulting in the disappearance of fine lines and wrinkles. At the same time, the laser’s heat evaporates damaged collagen. The skin tightens due to the heat, eliminating sagging skin and further reducing wrinkles.
Balancing Pigmentation
The laser disperses melanin in the epidermis, mitigating uneven pigmentation and fostering a more uniform skin tone.
Fixing Damage Done to Skin by UV Rays
The laser disperses melanin in the epidermis, mitigating uneven pigmentation and fostering a more uniform skin tone.
Precision Targeting of Concern Areas
In contrast to conventional plastic surgery methods such as facelifts, CO2 fractional laser therapy enables precise targeting of specific problem areas, preserving surrounding healthy skin tissues.
What to Expect After CO2 Laser Skin Resurfacing?
The downtime will vary depending on the patient and treatment. The healing process is different for everyone and certain skin types heal faster. The treatment intensity can differ based on your needs. The specific skin conditions will matter, as well.
The type of laser technology will also affect recovery times. CO2 laser skin resurfacing uses short pulsed light or continuous beam in a scanning pattern. This allows for precision when removing thin layers of skin. Recovery time for this type of treatment is usually around two weeks.
Fractional CO2 lasers may require less healing time. The fractional laser delivers narrow columns of light, so less skin is affected. The less skin damage you have, the less healing is necessary. Fractional CO2 lasers require about one week of recovery time.
Following the procedure, you might experience tightness, rawness, and increased sensitivity to sunlight on your skin. Additionally, swelling and discomfort may occur. Our team will furnish you with comprehensive aftercare instructions to alleviate pain and reduce inflammation. They will also guide you through the process of changing dressings and applying prescribed medication to the treated area.
Resurfacing treatment can be part of a more comprehensive skin care treatment plan, so the cost of CO2 laser therapy may also depend on the other treatments you receive.
What Influences the Average Cost of CO2 Laser Skin Resurfacing?
Laser treatment is a dynamic option that is effective for a variety of conditions. The goal of the treatment and the amount of skin surface treated might also affect the cost.
For example, dark circle laser treatment costs may differ from that of a laser treatment for wrinkles and blemishes. Acne scar laser treatment cost will be different from anti-aging care. Along those same lines, the cost of laser treatment for wrinkles cost will vary from varicose veins laser treatment cost.
The type of laser and area of the body can factor into the cost, as well. Full face skin resurfacing using an ablative laser might be priced differently than fractional CO2 laser cost. However, A fractional laser can provide a more targeted treated area. For instance, CO2 laser under eyes cost is worth it to reduce the risk of complications.
When considering the cost of treatment, the doctor will look at:
- The severity of the skin issues. For instance, deep wrinkles will require more intense laser treatment.
- The surface area of skin treated. Laser treatment for face cost may be different than that for the back based on surface area treated.
- The type of laser necessary to get the right results

Your dermatologist will create a skincare plan for you and review the various expenses, including if another cosmetic procedure might complement the treatment, such as BOTOX. You will know before the treatment what laser skin rejuvenation costs. They’ll break so you understand how much cellulite laser treatment costs and how much you pay to remove acne scars.
The CO2 laser treatment cost includes incidental expenses you might not consider upfront. The CO2 laser treatment expenses typically include:
- Facility fees
- Anesthesia
- Prescription medication costs
- Aftercare
- Market costs in the area
These all factor into the final CO2 laser price.
Is the Cost of CO2 Laser Skin Resurfacing Treatment Worth It?
Only you can answer that question, but laser treatment benefits are real and may be less than plastic surgery like a facelift. It can reduce fine lines, acne scarring, wrinkles, and damage from sun exposure. The therapy has a short recovery time and limited side effects.
Afterward, your skin will show reduced to no age spots or sun spots, have improved texture, and even have more elasticity. You will look and feel younger with bright, glowing skin.
Since insurance may not cover this treatment, consider what financing options are available to you and the interest rates involved, as well. Those fees should factor into any decision about affordability. Financing your treatment may add to the cost but improve accessibility for you.
Who Is a Good Candidate for CO2 Laser Skin Resurfacing Treatments?
Affordability isn’t the only thing that isn’t true with laser skin resurfacing treatments. Not everyone may be a candidate for such therapies. The ideal candidate will have:
- Acne or chickenpox scarring
- Uneven pigmentation
- Sun damage from frequent sunburns or years of not wearing sunscreen
- Uneven pigmentation
- Enlarged oil glands on the nose
- Fine lines on the face
- Skin cancer
- Rosacea
- Varicose veins on the face or chest
Consultation with your dermatologist can tell you if the treatment is good for your skincare needs.
Laser Skin Resurfacing at Venice Avenue Dermatology
Venice Avenue Dermatology offers the Nordlys system to provide cutting-edge laser technology for skin rejuvenation and the desired results.
The Nordlys system is FDA-approved and utilizes four primary elements for treatment:
- A narrowband Intense Pulsed Light (IPL) for minimal treatment risks compared to other laser options
- Two fractional non-ablative skin resurfacing technologies for fine lines, scars, and sun damage
- Nd:YAG 1064 nm laser technology for precise treatments
The Nordlys system provides comprehensive skin rejuvenation services in a professional, comfortable setting.
Venice Avenue also utilizes V-beam laser technology. The Vbeam laser technology is one of the most advanced pulsed-dye laser systems available—it treats vascular, pigmented, and non-pigmented lesions on the skin. This system is effective in conjunction with skin laser resurfacing procedures to enhance the results by targeting fine lines and acne scars.
Venice Avenue Dermatology offers other cosmetic and dermatology procedures, along with laser skin resurfacing. Our dedicated team and board-certified dermatologists can provide more detailed information on the costs of laser skin resurfacing at our Venice, Florida, office.
Since 1997, the healthcare professionals at Venice Avenue Dermatology have provided top-notch dermatology services for a variety of skin concerns, including laser skin resurfacing. Today, we offer state-of-the-art technology and personalized care plans. We are upfront about the costs and look to provide affordable plans for our clients regardless of their treatment needs at our location in Venice, Florida.
Frequently Asked Questions
There are two types: ablative, which treats continuous skin areas, and fractional, which targets specific areas more selectively.
Side effects may include swelling, redness, tightness, and increased sensitivity to sunlight. These are typically temporary and part of the healing process.
Yes, CO2 laser treatment can effectively treat varicose veins on the face and chest, improving their appearance.
Ablative lasers treat continuous skin areas, while fractional lasers target specific spots more selectively, leading to potentially shorter recovery times.
Generally, no. Since CO2 laser treatment is usually elective and not medically necessary, most insurance plans do not cover it.
The laser removes the outer skin layer and stimulates collagen production, leading to smoother and healthier skin texture.
Recovery time can range from a few days to several weeks, depending on the intensity of the treatment. Non-ablative lasers typically have shorter recovery times compared to ablative lasers.
Aftercare includes following specific instructions from your dermatologist, managing swelling and discomfort, and avoiding sun exposure to ensure proper healing.